
 It's reassuring to see that there are positive things one can do to maintain brain health as one ages. With normal aging, the brain typically shrinks a little with each passing decade - starting from about the age of 40. But one recent Australian study, which reviewed the results of many other studies, found that exercise slows down this shrinkage in humans, specifically in the left hippocampus. That is, that aerobic exercise had a significant positive effect on the volume of the left hippocampus. This matches the result of animal studies.
It's reassuring to see that there are positive things one can do to maintain brain health as one ages. With normal aging, the brain typically shrinks a little with each passing decade - starting from about the age of 40. But one recent Australian study, which reviewed the results of many other studies, found that exercise slows down this shrinkage in humans, specifically in the left hippocampus. That is, that aerobic exercise had a significant positive effect on the volume of the left hippocampus. This matches the result of animal studies.
The researchers pointed out that some studies found increases also in other parts of the human brain from exercise (e.g. in the white matter), but that they did not look at and review those studies. [See posts on research.] The good news is that positive effects were from exercise programs generally lasting less than 12 months. But it is unknown which type of exercise is best, or whether it is general "activity level and movement" that is most important. Bottom line: Get out there and move, move, move for brain health. And for cardiorespiratory fitness. It's all linked and it's all good. From Medical Xpress:
Exercise maintains brain size, new research finds
Aerobic exercise can improve memory function and maintain brain health as we age, a new Australian-led study has found. In a first of its kind international collaboration, researchers from Australia's National Institute of Complementary Medicine at Western Sydney University and the Division of Psychology and Mental Health at the University of Manchester in the UK examined the effects of aerobic exercise on a region of the brain called the hippocampus, which is critical for memory and other brain functions.
Brain health decreases with age, with the average brain shrinking by approximately five per cent per decade after the age of 40. Studies in mice and rats have consistently shown that physical exercise increases the size of the hippocampus but until now evidence in humans has been inconsistent.
The researchers systematically reviewed 14 clinical trials which examined the brain scans of 737 people before and after aerobic exercise programs or in control conditions. The participants included a mix of healthy adults, people with mild cognitive impairment such as Alzheimer's and people with a clinical diagnosis of mental illness including depression and schizophrenia. Ages ranged from 24 to 76 years with an average age of 66. The researchers examined effects of aerobic exercise, including stationary cycling, walking, and treadmill running. The length of the interventions ranged from three to 24 months with a range of 2-5 sessions per week.
Overall, the results – published in the journal NeuroImage– showed that, while exercise had no effect on total hippocampal volume, it did significantly increase the size of the left region of the hippocampus in humans.
"When you exercise you produce a chemical called brain-derived neurotrophic factor (BDNF), which may help to prevent age-related decline by reducing the deterioration of the brain," Mr Firth said. "Our data showed that, rather than actually increasing the size of the hippocampus per se, the main 'brain benefits' are due to aerobic exercise slowing down the deterioration in brain size. In other words, exercise can be seen as a maintenance program for the brain.".... Interestingly, physical exercise is one of the very few 'proven' methods for maintaining brain size and functioning into older age.

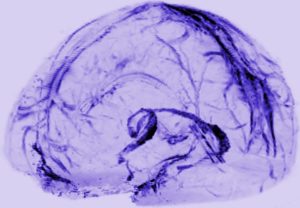 I can't resist posting excerpts from a recent article announcing that researchers just found an entirely new lymph system ("lymphatic vessels") in the brain that transports fluid in the brain, and is probably "crucial to metabolic and inflammatory processes". The image in this post shows the system in the brain. Amazing that it is only now "discovered" - apparently it was noticed by an anatomist 2 centuries ago, but this was pooh-poohed by modern day physicians. Until now. Excerpts from the Atlantic:
I can't resist posting excerpts from a recent article announcing that researchers just found an entirely new lymph system ("lymphatic vessels") in the brain that transports fluid in the brain, and is probably "crucial to metabolic and inflammatory processes". The image in this post shows the system in the brain. Amazing that it is only now "discovered" - apparently it was noticed by an anatomist 2 centuries ago, but this was pooh-poohed by modern day physicians. Until now. Excerpts from the Atlantic: For years studies have suggested that eating blueberries and other berries is good for our health (
For years studies have suggested that eating blueberries and other berries is good for our health ( Interesting study finding - that both high and low levels of magnesium is associated with a higher risk of dementia. Magnesium is an essential mineral needed for more than
Interesting study finding - that both high and low levels of magnesium is associated with a higher risk of dementia. Magnesium is an essential mineral needed for more than  Another article was published this month raising the issue of
Another article was published this month raising the issue of  Two studies looked at manganese and found that high levels are associated with problems. Manganese is an essential trace mineral necessary for development, metabolism, the antioxidant system, and for normal brain and nerve function. Getting manganese through foods (e.g. nuts, seeds, whole grains) is beneficial, but ing
Two studies looked at manganese and found that high levels are associated with problems. Manganese is an essential trace mineral necessary for development, metabolism, the antioxidant system, and for normal brain and nerve function. Getting manganese through foods (e.g. nuts, seeds, whole grains) is beneficial, but ing Should tackle football continue to be played in its current form? A
Should tackle football continue to be played in its current form? A  Lately more and more research has been finding health benefits with frequent consumption of extra virgin olive oil (EVOO). It is also a basic part of the popular Mediterranean diet - which emphasizes fresh fruits and vegetables, nuts, legumes (beans), whole grains, some fish, and extra virgin olive oil. Now a study conducted by investigators at Temple University in Philadelphia, Pennsylvania, suggests that the olive oil in the Mediterranean diet probably promotes healthy brain aging. The researchers said: "Our study is the first demonstration that EVOO can beneficially affect memory, amyloid plaques, and tau pathology, the hallmark lesions in the brain of Alzheimer's patients."
Lately more and more research has been finding health benefits with frequent consumption of extra virgin olive oil (EVOO). It is also a basic part of the popular Mediterranean diet - which emphasizes fresh fruits and vegetables, nuts, legumes (beans), whole grains, some fish, and extra virgin olive oil. Now a study conducted by investigators at Temple University in Philadelphia, Pennsylvania, suggests that the olive oil in the Mediterranean diet probably promotes healthy brain aging. The researchers said: "Our study is the first demonstration that EVOO can beneficially affect memory, amyloid plaques, and tau pathology, the hallmark lesions in the brain of Alzheimer's patients."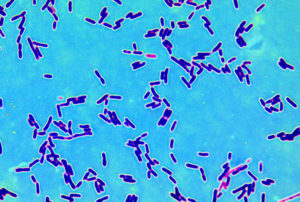 Could probiotics be used to treat depression? The medical site Medscape reported on a very small preliminary study (only 10 people) that tested that idea, with findings that suggested that taking certain probiotics does help treat the symptoms of mild to moderate depression. The bacteria taken were Lactobacillus helveticus and Bifidobacterium longum (in the product Probio'Stick). Specifically, the symptoms of mood, anhedonia (inability to feel pleasure), and sleep disturbance were significantly reduced after probiotoc therapy.
Could probiotics be used to treat depression? The medical site Medscape reported on a very small preliminary study (only 10 people) that tested that idea, with findings that suggested that taking certain probiotics does help treat the symptoms of mild to moderate depression. The bacteria taken were Lactobacillus helveticus and Bifidobacterium longum (in the product Probio'Stick). Specifically, the symptoms of mood, anhedonia (inability to feel pleasure), and sleep disturbance were significantly reduced after probiotoc therapy.