 Does vitamin D prevent cancer? There has been much debate over whether increasing levels of vitamin D (as measured in a person's blood) results in a lower incidence of cancer. Studies find a number of health problems linked to low levels of vitamin D (here, here, here), while studies looking at vitamin D and cancer have been "inconsistent" in their results. Some say yes - vitamin D is protective, while some say there is no effect from vitamin D supplements. Now a 4 year study (yes, yes - it's a very short length of time in which to study the onset of cancer) found no difference in the rate of cancer among two groups of postmenopausal women who received either: 2,000 IU per day of vitamin D3 and 1,500 mg per day of calcium OR an identical looking placebo. They looked for any kind of cancer occurring.
Does vitamin D prevent cancer? There has been much debate over whether increasing levels of vitamin D (as measured in a person's blood) results in a lower incidence of cancer. Studies find a number of health problems linked to low levels of vitamin D (here, here, here), while studies looking at vitamin D and cancer have been "inconsistent" in their results. Some say yes - vitamin D is protective, while some say there is no effect from vitamin D supplements. Now a 4 year study (yes, yes - it's a very short length of time in which to study the onset of cancer) found no difference in the rate of cancer among two groups of postmenopausal women who received either: 2,000 IU per day of vitamin D3 and 1,500 mg per day of calcium OR an identical looking placebo. They looked for any kind of cancer occurring.
The Creighton University researchers found a difference among the women after 4 years, with the vitamin D plus calcium supplement group having fewer cancers (and a lower percentage of cancer) as compared to the placebo group, but...it did not reach statistical significance. So you could say it was due to chance. But when the researchers looked at the number of cancers from year 2 to 4, then the difference was statistically significant - that vitamin D was protective. The researchers wonder if the cancers diagnosed in year 1 were already developing before the study started. Note: The 2,000 IU per day vitamin D3 supplements in this study are considered high doses - "high dose supplementation".
The researchers point out that the women who were given vitamin D3 and calcium supplements had a 30% lower risk of cancer, even though this difference in cancer incidence rates between the 2 groups did not quite reach statistical significance. But both groups started with a fairly high vitamin D level - an average 25-hydroxyvitamin D (25[OH]D) levels of 32.8 ng/m (which is above the average US population level). And in the supplement group it was raised to 43.9 ng/mL. Note that some researchers view vitamin D levels of 33 ng/mL (the baseline level in both groups) as already protective against cancer.
Also, even during the study the placebo group was allowed to take their own vitamin D and calcium supplements as long as it wasn't more than the recommended amounts (800 IU per day for vitamin D and 1500 mg per day for calcium) - which makes those individuals actually a low vitamin D supplementation group rather than no supplementation, which might hide any treatment effects and so make the results for the 2 groups look similar. What is needed is a much longer follow-up, larger groups of women, and both high and low dose vitamin D supplement groups. Some studies suggest that whether a low or high dose taken has an effect on cancer incidence.
I still think this study period was way too short - to me, 5 or more years would have been more convincing, and the groups too small. Also, it was unfortunate that they were also given calcium supplements or that there wasn't a just vitamin D group. Combining vitamin D with calcium supplements just muddies the results (in my opinion), and also because calcium supplements are linked to health problems such as cardiovascular disease. So in this study can't tell what the separate effects of calcium and vitamin D are. (Note that calcium rich foods, however, are beneficial to health.)
But a big positive of the study was that the women were randomly assigned to either the vitamin D plus calcium group or the placebo group, and no one - not the women or their doctors knew who got what until the end of the study (to eliminate bias it was "double-blind"). Note The supplements used were vitamin D3 and not D2. Vitamin D can also be easily obtained by exposure to sunlight in the summer months.
Excerpts from Creighton University release about the study in Science Daily: Does Vitamin D decrease risk of cancer?
The study, funded by the National Institutes of Health, is a randomized clinical trial of the effects of vitamin D supplementation on all types of cancer combined. The four-year study included 2,303 healthy postmenopausal women 55 years and older from 31 counties in Nebraska. Participants were randomly assigned to take either 2000 international units (IU) of vitamin D3 and 1500 mg. of calcium or identical placebos daily for 4 years. The vitamin D3 dose was about three times the US government's Recommended Dietary Allowance (RDA) of 600 IU for adults through age 70, and 800 IU for those 71 and older. Women who were given vitamin D3 and calcium supplements had 30% lower risk of cancer. This difference in cancer incidence rates between groups did not quite reach statistical significance. However, in further analyses, blood levels of vitamin D, specifically 25-hydroxyvitamin D (25(OH)D), were significantly lower in women who developed cancer during the study than in those who remained healthy.
Original study in JAMA: Effect of Vitamin D and Calcium Supplementation on Cancer Incidence in Older Women. Accompanying editorial about the study in JAMA: Vitamin D, Calcium, and Cancer: Approaching Daylight?

 Once again the Mediterranean diet is linked to health benefits - this time a 40% lower incidence of certain types of breast cancer in postmenopausal women. Following a Mediterranean style diet has been linked in earlier studies to various health benefits, such as lower rates of heart disease, lower rates of early death, and certain cancers.
Once again the Mediterranean diet is linked to health benefits - this time a 40% lower incidence of certain types of breast cancer in postmenopausal women. Following a Mediterranean style diet has been linked in earlier studies to various health benefits, such as lower rates of heart disease, lower rates of early death, and certain cancers. Another large study looking at screening mammograms for breast cancer has raised the issue of overdiagnosis and overtreatment once again. The purpose of mammography screening is to find cancer when it is small and so prevent cancer from growing and becoming advanced cancer. However, the researchers did not find this - there was a major increase in finding small cancers (the kind that may grow so slowly as to never cause any problems or that may even regress), but the rate of advanced cancers stayed the same.
Another large study looking at screening mammograms for breast cancer has raised the issue of overdiagnosis and overtreatment once again. The purpose of mammography screening is to find cancer when it is small and so prevent cancer from growing and becoming advanced cancer. However, the researchers did not find this - there was a major increase in finding small cancers (the kind that may grow so slowly as to never cause any problems or that may even regress), but the rate of advanced cancers stayed the same. More bad news about BPA (bisphenol A) - an
More bad news about BPA (bisphenol A) - an  Yikes! A good reason to lose weight now rather than years from now, and the importance of not ignoring a weight gain (you know, over the years as the pounds slowly creep up). The researchers found that for every 10 years of being overweight as an adult, there was an associated 7% increase in the risk for all obesity-related cancers. The degree of overweight (dose-response) during adulthood was important in the risk of developing cancer, especially for
Yikes! A good reason to lose weight now rather than years from now, and the importance of not ignoring a weight gain (you know, over the years as the pounds slowly creep up). The researchers found that for every 10 years of being overweight as an adult, there was an associated 7% increase in the risk for all obesity-related cancers. The degree of overweight (dose-response) during adulthood was important in the risk of developing cancer, especially for  Get active, really active, to reduce your risk for 5 diseases: breast cancer, colon cancer, heart disease, and ischemic stroke. Instead of the 150 minutes of brisk walking or 75 minutes per week of running (which is equal to the 600 metabolic equivalent (MET) minutes now recommended by the World Health Organization), this study found that much more exercise is needed for
Get active, really active, to reduce your risk for 5 diseases: breast cancer, colon cancer, heart disease, and ischemic stroke. Instead of the 150 minutes of brisk walking or 75 minutes per week of running (which is equal to the 600 metabolic equivalent (MET) minutes now recommended by the World Health Organization), this study found that much more exercise is needed for 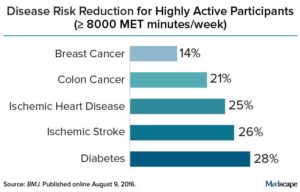 Credit: Medscape
Credit: Medscape Amazing! Researchers found that the bacteria found in breast cancer patients and healthy patients are different. (
Amazing! Researchers found that the bacteria found in breast cancer patients and healthy patients are different. ( Surprising results (to me at least) from research comparing various diets and incidence of several cancers in 11,082 individuals in the Netherlands over a 20 year period. I expected the daily meat eaters to have higher rates of the 3 cancers studied, but no....
Surprising results (to me at least) from research comparing various diets and incidence of several cancers in 11,082 individuals in the Netherlands over a 20 year period. I expected the daily meat eaters to have higher rates of the 3 cancers studied, but no....