 As we know, chronic inflammation is linked to cancer and other diseases. It is long-term persistent low-grade inflammation, and it has a "wear and tear" effect on the body. What causes chronic inflammation? Being overweight or obese, sedentary lifestyle, Western (low fiber, high processed foods and meat) diet, chronic illnesses, viruses or bacteria (e.g., gum disease), smoking, air pollution, stress, excessive alcohol intake. It often does not have symptoms, but doctors can test for C-reactive protein levels (CRP), which increase when the body is inflamed. So you absolutely want to lower chronic inflammation if you can.
As we know, chronic inflammation is linked to cancer and other diseases. It is long-term persistent low-grade inflammation, and it has a "wear and tear" effect on the body. What causes chronic inflammation? Being overweight or obese, sedentary lifestyle, Western (low fiber, high processed foods and meat) diet, chronic illnesses, viruses or bacteria (e.g., gum disease), smoking, air pollution, stress, excessive alcohol intake. It often does not have symptoms, but doctors can test for C-reactive protein levels (CRP), which increase when the body is inflamed. So you absolutely want to lower chronic inflammation if you can.
High dietary intake of fruits and vegetables, which are rich in polyphenols, has been linked through many studies with reduced risk for diseases that are associated with chronic inflammation, such as cardiovascular disease, type II diabetes, cancers, Alzheimer’s disease, and Parkinson’s disease. Polyphenols are a class of chemicals or micronutrients found in many foods, especially fruits and vegetables.
New research looked at 31 polyphenols (alone and in some mixtures) to see which lowered inflammation the most. They found that some mixtures of polyphenols actually had more than an additive effect - that it's more than a sum of the individual polyphenols. They found that the polyphenols resveratrol, isorhamnetin, and curcumin were the most anti-inflammatory. Isorhamnetin is a flavonol that occurs in apples, onions and green tea; curcumin is from the Indian spice turmeric; and resveratrol is present in the skin of red, purple and black grapes, and in especially high concentrations in Itadori tea (from Japanese knotweed). Another important anti-inflammatory polyphenol is vanillic acid, which is found in vanilla, wine, whole wheat, and berries.
Just remember that it is better to eat a variety of fruits and vegetables rather than taking supplements. Foods are more than just one or 2 isolated ingredients, but consist of many micronutrients, microbes, etc , and when eating a varied diet, a person typically has mixtures of many polyphenols in their system at once. The research finds that these polyphenol mixtures interact with one another. Studies typically find real foods to be superior to supplements in beneficial health effects. From Science Daily:
What foods can help fight the risk of chronic inflammation?
A new study by the University of Liverpool's Institute of Ageing and Chronic Disease has identified food stuffs that can help prevent chronic inflammation that contributes to many leading causes of death. Inflammation occurs naturally in the body but when it goes wrong or goes on too long, it can trigger disease processes. Uncontrolled inflammation plays a role in many major diseases, including cancer, heart disease, diabetes and Alzheimer's disease.
Diets rich in fruits and vegetables, which contain polyphenols, protect against age-related inflammation and chronic diseases. Polyphenols are abundant micronutrients in our diet, and evidence for their role in the prevention of degenerative diseases such as cancer and cardiovascular diseases is already emerging. The health effects of polyphenols depend on the amount consumed and on their bioavailability.
T-cells, or T-lymphocytes, are a type of white blood cell that circulate around our bodies, scanning for cellular abnormalities and infections. They contribute to cell signalling molecules (cytokines) that aid cell-to-cell communication in immune responses and stimulate the movement of cells towards sites of inflammation, infection and trauma. Cytokines are modulated by fruit and vegetable intake.
The study, conducted by Sian Richardson and Dr Chris Ford from the University's Institute of Ageing and Chronic Disease, examined the different potencies of the polyphenols. Sian Richardson, said: "The results of our study suggest that (poly)phenols derived from onions, turmeric, red grapes, green tea and açai berries may help reduce the release of pro-inflammatory mediators in people at risk of chronic inflammation. "Older people are more susceptible to chronic inflammation and as such they may benefit from supplementing their diets with isorhamnetin, resveratrol, curcumin and vanillic acid or with food sources that yield these bioactive molecules."

 Great article about cancer and sugar. Yes, there is more and more research recently finding a connection with sugar, raised insulin levels, and cancer (as in sugar feeds cancer). Do go read it. Some excerpts from the May 15 Sunday magazine of the NY Times:
Great article about cancer and sugar. Yes, there is more and more research recently finding a connection with sugar, raised insulin levels, and cancer (as in sugar feeds cancer). Do go read it. Some excerpts from the May 15 Sunday magazine of the NY Times: Did you ever wonder about all the consumer products that have fragrances in them and whether they are safe to use? Think of all the fragrances in personal care products and perfumes, in air fresheners, scented soaps, cleaning products, scented candles, even laundry detergents, and scented dryer sheets.
Did you ever wonder about all the consumer products that have fragrances in them and whether they are safe to use? Think of all the fragrances in personal care products and perfumes, in air fresheners, scented soaps, cleaning products, scented candles, even laundry detergents, and scented dryer sheets. For the first time ever, one type of cancer has been reclassified as a non-cancer. An international panel of pathologists and clinicians has reclassified a type of thyroid cancer to reflect that it is noninvasive and has a low risk for recurrence.The panel renamed encapsulated follicular variant of papillary thyroid carcinoma (EFVPTC) as noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP). There has been concern for a while of the costs (financial, physical, and mental) of the overdiagnosis and overtreatment for something that won't spread (it's "indolent" and "low-risk").
For the first time ever, one type of cancer has been reclassified as a non-cancer. An international panel of pathologists and clinicians has reclassified a type of thyroid cancer to reflect that it is noninvasive and has a low risk for recurrence.The panel renamed encapsulated follicular variant of papillary thyroid carcinoma (EFVPTC) as noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP). There has been concern for a while of the costs (financial, physical, and mental) of the overdiagnosis and overtreatment for something that won't spread (it's "indolent" and "low-risk"). Coffee consumption overall seems to be beneficial to health in various ways, such as lowering the risk of colorectal cancer. But there are times one should limit how much one drinks, such as during the
Coffee consumption overall seems to be beneficial to health in various ways, such as lowering the risk of colorectal cancer. But there are times one should limit how much one drinks, such as during the  Nice summary article about the known benefits of nuts and seeds, and the nutrients they contain. Bottom line: all nuts and seeds are beneficial to health. It's best to eat a variety of nuts, and eat some nuts daily or at least a few times a week. A typical serving is 1/4 cup or small handful of nuts. Go to the article for the complete nut and seed list and a nut and seed nutrient chart. From Today's Dietician:
Nice summary article about the known benefits of nuts and seeds, and the nutrients they contain. Bottom line: all nuts and seeds are beneficial to health. It's best to eat a variety of nuts, and eat some nuts daily or at least a few times a week. A typical serving is 1/4 cup or small handful of nuts. Go to the article for the complete nut and seed list and a nut and seed nutrient chart. From Today's Dietician: A recent
A recent 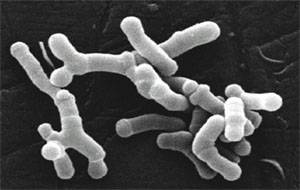 The possibility of giving microbes in the future (whether bacteria, viruses, or fungi) to treat cancer is amazing. Of course big pharma is pursuing this line of research, which is called immunotherapy (stimulating the body's ability to fight tumors). The Bloomberg Business article discusses a number of big pharma companies entering the field and their main focus. The study in the journal Science finding that giving common beneficial bacteria (Bifidobacterium breve and Bifidobacterium longum) to mice to slow down melanoma tumor growth is a first step. The researchers themselves said that the 2 common beneficial bacteria species exhibited anti-tumor activity in the mice and was as effective as an immunotherapy in controlling the growth of skin cancer. But note that the bacteria needed to be live. Stay tuned....
The possibility of giving microbes in the future (whether bacteria, viruses, or fungi) to treat cancer is amazing. Of course big pharma is pursuing this line of research, which is called immunotherapy (stimulating the body's ability to fight tumors). The Bloomberg Business article discusses a number of big pharma companies entering the field and their main focus. The study in the journal Science finding that giving common beneficial bacteria (Bifidobacterium breve and Bifidobacterium longum) to mice to slow down melanoma tumor growth is a first step. The researchers themselves said that the 2 common beneficial bacteria species exhibited anti-tumor activity in the mice and was as effective as an immunotherapy in controlling the growth of skin cancer. But note that the bacteria needed to be live. Stay tuned....