 News about the controversial pesticide Roundup and its active ingredient glyphosate just keep coming. Roundup is the most heavily used pesticide in the world, and it is used as a herbicide or weed-killer throughout the USA. Its use is rapidly rising, especially due to its use for preharvest applications on crops, and for genetically modified Roundup Ready crops. The chemical giant Monsanto (manufacturer of Roundup) insists that Roundup is safe for humans and the environment, but studies are indicating otherwise (see posts on Roundup). And yes, the pesticide and its residues are found wherever its presence is looked for. So one very important question is: If this heavily used pesticide is found in the foods we eat, and is around us (thus we have chronic low levels of exposure), what is it doing to us, if anything?
News about the controversial pesticide Roundup and its active ingredient glyphosate just keep coming. Roundup is the most heavily used pesticide in the world, and it is used as a herbicide or weed-killer throughout the USA. Its use is rapidly rising, especially due to its use for preharvest applications on crops, and for genetically modified Roundup Ready crops. The chemical giant Monsanto (manufacturer of Roundup) insists that Roundup is safe for humans and the environment, but studies are indicating otherwise (see posts on Roundup). And yes, the pesticide and its residues are found wherever its presence is looked for. So one very important question is: If this heavily used pesticide is found in the foods we eat, and is around us (thus we have chronic low levels of exposure), what is it doing to us, if anything?
This month the results of a study of 69 pregnant women receiving prenatal care at an Indiana obstetric practice was presented at a Children’s Environmental Health Network (CEHN) conference. The researchers reported that they found the presence of glyphosate and its breakdown products (aminomethylphosphonic acid or AMPA) in the urine of 91% of pregnant women. They found that higher levels of glyphosate were associated with lower than average birth weights and shorter pregnancy length (gestation age). Also, women living in rural areas had higher average glyphosate levels than women in urban/suburban regions. The researches suggested that it was because the rural women lived close to corn and soybean fields where glyphosate is heavily used.
The researchers also pointed out that this is especially worrisome because low birth weights and shortened pregnancy length (gestation) are seen as risk factors for many health and neurodevelopmental problems over the course of an individual’s life - lower cognitive abilities (including IQ), diabetes, heart disease, high blood pressure, and obesity. Of course the researchers plan to expand this research on more women.
But unfortunately US government agencies such as the FDA are not testing for the presence of glyphosate residues in foods (a major way we are exposed to glyphosate), even though they test for many other pesticides. So testing for the most heavily used pesticide in the world in foods is deliberately not being done! It doesn't matter whether one thinks that Roundup (glyphosate) is harmful or not - we should know what foods this pesticide in the world appears in and at what levels. So far, whatever conventional foods are looked at, glyphosate residues are found. Even foods that one does not expect it in, such as honey. On the other hand, organic foods or crops are not allowed to use Roundup or glyphosate, so eating organic foods is the only way to avoid the pesticide. And of course, by not using Roundup or other glyphosate products on the property where you live.
The researchers and CEHN (Children’s Environmental Health Network) have put together a web-site documenting the increase in Roundup (glyphosate) use in the United States in the past few decades and why we should be concerned. There are many links at the thorough and well-researched site. If one looks at only a few pages, then look at the introduction page - The Project, the Birth Outcomes section, and the Biomonitoring Data page - which discusses "biomonitoring" to track levels of chemicals such as pesticides in human urine and blood, and why we should be concerned. They also discuss 2,4-D - another popular pesticide (herbicide or weed-killer), which is also used in many lawn "weed and feed" products. 2.4-D has serious health concerns, but its use is also rapidly increasing on farms due the increase in genetically modified crops (which allow it to be sprayed on crops without killing the crops).
Bottom line: We are being exposed to chronic low levels of pesticides in our environment and foods - and we really don't know what this is doing to us. We don't even know the extent of our exposures because it is not being measured. This is especially worrisome because our exposure to some of these pesticides is rapidly increasing.
From the investigative journalism site FERN: Researchers find glyphosate in pregnant women, worry about impact on infants
A team of scientists this week released early results of an ongoing study spotlighting concerns about the rising use of pesticides and reproductive risks to women and children. The researchers tested and tracked, over a period of two years, the presence of the common herbicide glyphosate in the urine of 69 expectant mothers in Indiana.
The team – led by Paul Winchester, medical director of the neonatal intensive care unit at the Franciscan St. Francis Health System and professor of clinical pediatrics at Riley Hospital for Children in Indianapolis, Ind. – found glyphosate residues in 91 percent of the women, and high levels of those residues appeared to correlate with shortened pregnancies and below-average birth weights adjusted for age. The findings alarmed the researchers because such babies are at increased risk of diabetes, heart disease, high blood pressure, and lower cognitive abilities. “Gestational age maximizes the size of your brain at birth, and any shortening is essentially a reduction of IQ points,” Winchester said in an interview with FERN’s Ag Insider. “It has not just health, but lifetime achievement implications.”
This is the first time that anyone has demonstrated glyphosate is present in pregnant women in the U.S., according to Winchester. However, the results were limited by a small sample size. He and his colleagues plan to submit their research to a peer-reviewed journal within the month and they hope to expand the study later this year. “The fact that we were able to find adverse effects on the small number of people we measured would imply a larger study is needed immediately to find out if this is prevalent everywhere,” Winchester says. “This is a critical piece of information that I think people should be concerned about.”
Glyphosate is the world’s most popular herbicide and the key ingredient in Monsanto’s Roundup weed killer. Globally, 9.4 million tons of glyphosate have been sprayed on crops, lawns, and gardens since the chemical was released on the market in 1974....Currently, concerns about the safety of glyphosate are at the center of a major national lawsuit. Monsanto is being sued by hundreds of U.S. consumers who say the company did not warn them, despite evidence, that the chemical can cause cancers such as non-Hodgkin lymphoma, a blood disease. A key piece of testimony in the suit is a 2015 International Agency for Research on Cancer (IARC) report stating that glyphosate is “probably carcinogenic to humans.” Monsanto contests the listing, citing rulings by the EPA, the European Chemicals Agency, and the European Food Safety Authority that did not find cancer risks.
Winchester has long studied the risks posed by agrochemicals, finding in a 2009 study that high levels of the farming chemical atrazine in water was associated with increased risk of genital birth defects in children. In the glyphosate study, Winchester and his colleagues considered whether water might again be the exposure route for the pregnant women they monitored. After testing water samples, the scientists concluded that it was not the source. They suspect diet may play a role. The Food and Drug Administration, however, recently suspended the testing of glyphosate residues in food, citing the need for improved validation methods.
Experts say the spread of weeds resistant to glyphosate in the Midwest is triggering intensification of herbicide use over longer periods of time. “Until this year, most herbicides in the Midwest were sprayed during a six-week window, but now heavy herbicide spray season will last at least four months, placing more women and children at heightened risk,” Phil Landrigan, dean for global health at Mount Sinai Medical School and a member of the research team, said in a statement. As a result, he and his colleagues predict the risk of reproductive problems and adverse birth outcomes will rise among women and children living in rural areas.
Another article on this research is from Carey Gillam for Huffington Post: Moms Exposed To Monsanto Weed Killer Means Bad Outcomes For Babies
Chocolate lovers can rejoice - because another study, which was actually a review of other studies - found that frequent consumption of chocolate, cocoa, and cocoa flavanols (an ingredient of cocoa) is linked with beneficial health effects. These included cardiovascular benefits, and dose-dependent improvements in cognition, attention, and memory. In other words - the more frequently one eats chocolate and cocoa (especially dark chocolate), the more beneficial health effects. So eat and enjoy! From Medical Xpress:

 Hah! Another study showing that YES, older adults have sex, and that more frequent sexual activity (as in at least weekly vs never or only monthly) may also be good for the brain and brain function in older adults. 73 people between the ages of 50 and 83 participated
Hah! Another study showing that YES, older adults have sex, and that more frequent sexual activity (as in at least weekly vs never or only monthly) may also be good for the brain and brain function in older adults. 73 people between the ages of 50 and 83 participated  Many of us who who spend time outdoors worry about ticks. Just about everyone in the Northeast knows someone who has struggled with Lyme disease or one of the other diseases spread by ticks. An earlier
Many of us who who spend time outdoors worry about ticks. Just about everyone in the Northeast knows someone who has struggled with Lyme disease or one of the other diseases spread by ticks. An earlier  News about the controversial pesticide Roundup and its active ingredient glyphosate just keep coming. Roundup is the most heavily used pesticide in the world, and it is used as a
News about the controversial pesticide Roundup and its active ingredient glyphosate just keep coming. Roundup is the most heavily used pesticide in the world, and it is used as a  An interesting study looked at what the act of walking does to our brain, and found that it can modify and increase the amount of blood that’s sent to the brain (which is viewed as
An interesting study looked at what the act of walking does to our brain, and found that it can modify and increase the amount of blood that’s sent to the brain (which is viewed as  This post is more on the theme of nanoparticles and human health. My
This post is more on the theme of nanoparticles and human health. My  Image of magnetite nanoparticles from the exhaust plume of a diesel engine. Credit Maher et al study, 2016.
Image of magnetite nanoparticles from the exhaust plume of a diesel engine. Credit Maher et al study, 2016.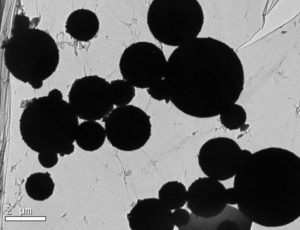 A microscopic image shows magnetite nanoparticles in the human brain. Barbara Maher et al study, 2016.
A microscopic image shows magnetite nanoparticles in the human brain. Barbara Maher et al study, 2016. Another study has linked childhood behavioral problems to pesticide exposure, this time to pyrethroid insecticide exposure. Pyrethroids are synthetic pesticides (insecticides) that are increasingly used for personal use (mosquito repellents and treatments for head lice, scabies), on pets (for fleas), home use (e.g., Raid pesticides), and in agriculture.
Another study has linked childhood behavioral problems to pesticide exposure, this time to pyrethroid insecticide exposure. Pyrethroids are synthetic pesticides (insecticides) that are increasingly used for personal use (mosquito repellents and treatments for head lice, scabies), on pets (for fleas), home use (e.g., Raid pesticides), and in agriculture. A study found that daily drinking of tea (either black tea/oolong or green tea) is associated with a lower risk of "neurocognitive disorders" - in cognitive impairment in women, and in a lower risk of Alzheimer's disease in both men and women who are genetically predisposed to the disease (apolipoprotein E (APOE) genotype) - when compared to those who never or rarely drank tea. The researchers called long-term daily tea drinking as "neuroprotective".
A study found that daily drinking of tea (either black tea/oolong or green tea) is associated with a lower risk of "neurocognitive disorders" - in cognitive impairment in women, and in a lower risk of Alzheimer's disease in both men and women who are genetically predisposed to the disease (apolipoprotein E (APOE) genotype) - when compared to those who never or rarely drank tea. The researchers called long-term daily tea drinking as "neuroprotective". A new study was published that supports eating lots of blueberries (or drinking blueberry juice) for health - this time better brain functioning in people aged 65 to 77 who drank concentrated blueberry juice daily for 12 weeks. The people randomly assigned to the group drinking blueberry juice daily showed improvements in cognitive function, blood flow to the brain, and activation of the brain while carrying out cognitive tests. The people received MRIs (magnetic resonance imaging), as well as various blood tests and cognitive tests.
A new study was published that supports eating lots of blueberries (or drinking blueberry juice) for health - this time better brain functioning in people aged 65 to 77 who drank concentrated blueberry juice daily for 12 weeks. The people randomly assigned to the group drinking blueberry juice daily showed improvements in cognitive function, blood flow to the brain, and activation of the brain while carrying out cognitive tests. The people received MRIs (magnetic resonance imaging), as well as various blood tests and cognitive tests.