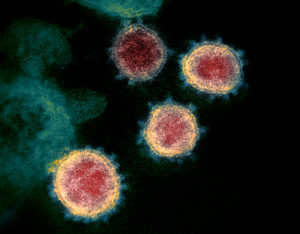
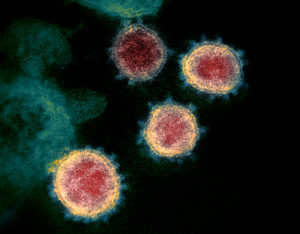
 Covid-19 is a weird and scary virus. It turns out that while most people report none or minimal symptoms from a Covid-19 infection, there are also thousands of people reporting prolonged symptoms. Instead of being sick with Covid-19 for 2 weeks or so (the average for mild cases), they get sick with the viral infection and then it never seems to go away. There may be big ups and downs with a wide variety of serious symptoms (including neurological and gastrointestinal symptoms, fatigue, fevers, heart palpitations), but they are still sick weeks or months after the initial infection.
Covid-19 is a weird and scary virus. It turns out that while most people report none or minimal symptoms from a Covid-19 infection, there are also thousands of people reporting prolonged symptoms. Instead of being sick with Covid-19 for 2 weeks or so (the average for mild cases), they get sick with the viral infection and then it never seems to go away. There may be big ups and downs with a wide variety of serious symptoms (including neurological and gastrointestinal symptoms, fatigue, fevers, heart palpitations), but they are still sick weeks or months after the initial infection.
What is going on? People experiencing long-term Covid-19 symptoms refer to themselves as "long-haulers" or "long-termers". Covid-19 is a new and complex disease that seems to attack many organs of the body. It is such a new disease that much is still unknown, including why some people seem to experience Covid-19 symptoms for weeks or months after the initial infection. But some possibilities are emerging, such as myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) . ME/CFS clusters have occurred in the past after many infectious outbreaks, including after the SARS epidemic (a similar coronavirus) of 2003.
Paul Garner, professor of infectious diseases at Liverpool School of Tropical Medicine, has documented his battle with long-term Covid-19 symptoms in the British Medical Journal blog (also June 23 follow-up), and the need for "pacing" during recovery to prevent relapses. [twitter.com/paulgarnerwoof?lang=en ]
There are support groups on Facebook such as Survivor Corps, Covid-19 Support Group (have it/had it), Long Covid Support Group, and Long Haul Covid Fighters. Fiona Lowenstein started a Covid-19 support group (Body Politic Covid-19 support group) for people living with the virus
Bottom line: Don't let others, including doctors, dismiss your symptoms. They are real. Read about the experiences of others and join support groups. The good news is that slowly, over time, most people are reporting improvement. Unfortunately, it will take time for public health officials, including the CDC, to catch up and acknowledge what people are already experiencing.
The following are some good articles to read. Start with Ed Yong's article in The Atlantic: Covid-19 Can Last for Several Months
A first person account of prolonged Covid-19 symptoms. Professor Paul Garner's original British Medical Journal (BMJ) piece for the BMJ blog: Paul Garner: For 7 weeks I have been through a roller coaster of ill health, extreme emotions, and utter exhaustion
From VOX, the site for explanatory journalism: The emerging long-term complications of Covid-19, explained
From VOX: My coronavirus survivor group is my most important medical support right now
The CDC view of ME/CFS (but with no mention of Covid-19). From the Centers For Disease Control and Prevention (CDC): Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)
 Holy mackerel! Currently COVID-19 kills someone in the United States every 107 seconds! And the U.S. is reporting more than 70,000 new coronavirus cases each day.
Holy mackerel! Currently COVID-19 kills someone in the United States every 107 seconds! And the U.S. is reporting more than 70,000 new coronavirus cases each day.
 Today while waiting in a line at the store, everyone wearing the required masks, the woman in front of me told me that the masks are useless and that there isn't good evidence that the coronavirus is spread through the air. Huh? Where did she get that idea? Of course there is airborne transmission of the virus!
Today while waiting in a line at the store, everyone wearing the required masks, the woman in front of me told me that the masks are useless and that there isn't good evidence that the coronavirus is spread through the air. Huh? Where did she get that idea? Of course there is airborne transmission of the virus! Several studies are now suggesting that
Several studies are now suggesting that  Worrisome news: having a COVID-19 infection during pregnancy may be injuring the placenta, even if the pregnant woman has no symptoms (asymptomatic) and the baby appears healthy at birth. The human placenta is the temporary organ that nourishes and maintains the developing fetus during pregnancy. It provides oxygen and nutrients to the baby, and removes waste products.
Worrisome news: having a COVID-19 infection during pregnancy may be injuring the placenta, even if the pregnant woman has no symptoms (asymptomatic) and the baby appears healthy at birth. The human placenta is the temporary organ that nourishes and maintains the developing fetus during pregnancy. It provides oxygen and nutrients to the baby, and removes waste products. Have you recently lost your sense of taste or smell? Then you may be infected with the coronavirus COVID-19, even if you don't display any other symptoms.
Have you recently lost your sense of taste or smell? Then you may be infected with the coronavirus COVID-19, even if you don't display any other symptoms.