
A recent study confirmed that in the skin condition called rosacea, the skin microbiome is out of whack (dysbiosis). Of course. The study also confirmed that treatment with a topical ivermectin cream helps with the inflamed red skin rashes on the face and lowers the number of Demodex mites found on the skin.
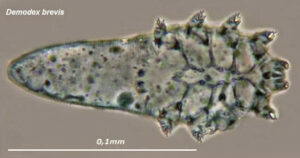
But while the cream improved symptoms in 44% of the patients, it didn't correct the skin dysbiosis. In rosacea, there is a big increase of Demodex mites (compared to normal levels) at the site of the red rashes or lesions. After the topical ivermectin cream treatment, the number of mites decreased in 88% of the rosacea group to more normal levels. [Yes, we all have Demodex mites living on our skin.]
However, other bacterial species are still different in the rosacea group compared to healthy persons without rosacea. The researchers found Cutibacterium species are predominant in healthy persons without rosacea, but are not found in persons when they have rosacea inflammation. Instead Staphylococcus species take over (just like in atopic dermatitis).
The skin microbiome is the community of bacteria, viruses, fungi that live on our skin. Rosacea is an inflammatory skin condition that typically affects the face resulting in redness, pimples, swelling, and dilated blood vessels. It frequently begins with flushing (redness) of the face in symmetrical patches, and it may or may not progress.
Excerpts from the medical site Medscape: Topical Ivermectin Study Sheds Light on Dysbiosis in Rosacea
Topical ivermectin has significant clinical efficacy and decreases the density of Demodex mites found in the skin of people with rosacea, but cutaneous dysbiosis remains, according to a report presented at the recent European Academy of Dermatology and Venereology (EADV) 2023 Congress. ...continue reading "The Skin Microbiome Is Different In Persons With Rosacea"




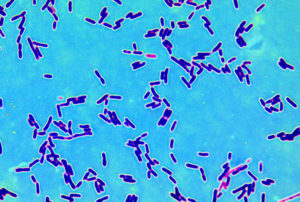
 Ever wonder what bacteria are living on your kitchen surfaces, including sponges? It turns out that even with different hygiene, dietary habits, and cooking practices, there is a core group of bacteria that are common to all kitchen surfaces (core microbiota). At least this was true for residential kitchens in 5 European countries.
Ever wonder what bacteria are living on your kitchen surfaces, including sponges? It turns out that even with different hygiene, dietary habits, and cooking practices, there is a core group of bacteria that are common to all kitchen surfaces (core microbiota). At least this was true for residential kitchens in 5 European countries.

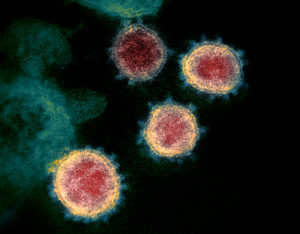
 The more physically active a person is before getting COVID-19, the lower the rates of hospitalization, deterioration events, and death from COVID-19 infection. In other words, physical activity is protective.
The more physically active a person is before getting COVID-19, the lower the rates of hospitalization, deterioration events, and death from COVID-19 infection. In other words, physical activity is protective. We all know that microbes (fungi, viruses, bacteria) live throughout our bodies - this is the human microbiome or microbiota. What is really interesting is that cancer tumors also have microbiomes (tumor microbiome), and these microbial communities are different than that found in healthy people (without tumors).
We all know that microbes (fungi, viruses, bacteria) live throughout our bodies - this is the human microbiome or microbiota. What is really interesting is that cancer tumors also have microbiomes (tumor microbiome), and these microbial communities are different than that found in healthy people (without tumors).