 Once again a study (this time a review and meta-analysis of other studies) found an alarming and steep decline in sperm counts in men from Western countries over a 40 year period. This steep decline for both sperm concentration (SC) and total sperm count (TSC) is for men in North America, Europe, Australia, and New Zealand. The sperm count and sperm concentration declined 50 to 60% in the period between 1973 to 2011 - with a downward slope showing a decline of -1.4% to -1.6% per year. On the other hand, men from South America, Asia and Africa did not show a decline.
Once again a study (this time a review and meta-analysis of other studies) found an alarming and steep decline in sperm counts in men from Western countries over a 40 year period. This steep decline for both sperm concentration (SC) and total sperm count (TSC) is for men in North America, Europe, Australia, and New Zealand. The sperm count and sperm concentration declined 50 to 60% in the period between 1973 to 2011 - with a downward slope showing a decline of -1.4% to -1.6% per year. On the other hand, men from South America, Asia and Africa did not show a decline.
The authors of the study were very concerned over the results showing this decline in Western countries, with no evidence of the decline leveling off. As these declines continue, more and more men will have sperm counts below the point at which they can reproduce. Instead they will be infertile or "sub-fertile" (with a decreased probability of conceiving a child). The threshold level associated with a "decreased monthly probability of conception" is considered to be 40 million/ml.
Shockingly - this study found that in 1973 when Western men who were not selected for fertility, and didn't know their fertility status (e.g., college students, men screened for the military) - the average sperm concentration was 99 million/ml, but by 2011 it was 47.1 million/ml. These men were called "unselected" and are likely to be representative of men in the general population. Men known to be fertile (e.g., had fathered a child) were at 83.8 million/ml in 1976, but were down to 62.0 million/ml in 2011. Both groups had consistent declines year after year.
What about the men from South America, Asia, and Africa? There, studies showed that the "unselected" men (not selected for fertility and who didn't know their fertility status) started out at 72.7 million/ml in 1983, and were at 62.6 million/ml in 2011, while men known to be fertile started out on average at 66.4 million/ml in 1978 and were at 75.7 million/ml in 2011. They did not show the decline of the North American, European, Australian, and New Zealand group of men.
What does this mean? And what is going on? These results go beyond fertility and reproduction. The decline is consistent with other male reproductive health indicators over the last few decades: higher incidence of testicular cancer, higher rates of cryptorchidism, earlier onset of male puberty, and decline in average testosterone levels. Instead, it appears that sperm counts of men are "the canary in the mine" for male health - evidence of harm to men from environmental and lifestyle influences.
These Western developed countries are awash in chemicals and plastics, also with endocrine disruptors (hormone disruptors) in our foods, our personal care products, etc - and so studies find these chemicals in all of us (in varying degrees). Same with flame retardants, pesticides, "scented" products. Exposure to all sorts of environmental pollutants - whether in air, water, soil, our food - such as high levels of aluminum. All of these can have an effect on sperm counts and reproductive health.
And note that chemicals that can depress sperm counts are also linked to many health problems, including chronic diseases.
What can you do? You can lower your exposure to many chemicals (e.g., pesticides), plastics, and endocrine disruptors, but you can't avoid them totally. Yes, it'll mean reading labels and ingredient lists on foods, personal care products (such as soaps, shampoo, lotion), and products used in the home. [LIST OF THINGS YOU CAN EASILY DO]
TRY TO AVOID OR LOWER EXPOSURE TO: phthalates, parabens, BPA, BPS, and even BPA-free labeled products (all use similar chemicals), flame-retardants (e.g., in upholstered furniture and rugs), stain-resistant, dirt-resistant, waterproof coatings, Scotchgard, non-stick cookware coatings, dryer sheets, scented products (including scented candles and air fresheners), fragrances, pesticides in the yard and home, and "odor-free", antibacterial, antimicrobial, anti-mildew products. Don't microwave foods in plastic containers (including microwave popcorn bags).
INSTEAD: Try to eat more organic foods, look for organic or least-toxic Integrated Pest Management (IPM) alternatives for the home and garden. Store foods as much as possible in glass, ceramic, or stainless steel containers. Buy foods, if possible, that are in glass bottles - not cans (all lined with endocrine disrupting chemicals) and not plastic bottles or containers (plastics leach). Some people use water filters because there are so many contaminants in our water, even if they meet federal guidelines on "allowable levels" in the water.
Avoid cigarette smoke or smoking. Try to lose weight if overweight. Open windows now and then in your residence to lower indoor air pollution. The list is long - yes, a lifestyle change! (see posts on ENDOCRINE DISRUPTORS, FLAME RETARDANTS, and PESTICIDES)
From Medical Xpress: Study shows a significant ongoing decline in sperm counts of Western men
In the first systematic review and meta-analysis of trends in sperm count, researchers from the Hebrew University-Hadassah Braun School of Public Health and Community Medicine and the Icahn School of Medicine at Mount Sinai report a significant decline in sperm concentration and total sperm count among men from Western countries.
By screening 7,500 studies and conducting a meta-regression analysis on 185 studies between 1973 and 2011, the researchers found a 52.4 percent decline in sperm concentration, and a 59.3 percent decline in total sperm count, among men from North America, Europe, Australia and New Zealand who were not selected based on their fertility status. In contrast, no significant decline was seen in South America, Asia and Africa, where far fewer studies have been conducted. The study also indicates the rate of decline among Western men is not decreasing: the slope was steep and significant even when analysis was restricted to studies with sample collection between 1996 and 2011.
The findings have important public health implications. First, these data demonstrate that the proportion of men with sperm counts below the threshold for subfertility or infertility is increasing. Moreover, given the findings from recent studies that reduced sperm count is related to increased morbidity and mortality, the ongoing decline points to serious risks to male fertility and health.
"Decreasing sperm count has been of great concern since it was first reported twenty-five years ago. This definitive study shows, for the first time, that this decline is strong and continuing. The fact that the decline is seen in Western countries strongly suggests that chemicals in commerce are playing a causal role in this trend," Dr. Shanna H Swan, a professor in the Department of Environmental Medicine and Public Health at the Icahn School of Medicine at Mount Sinai, New York.
While the current study did not examine causes of the observed declines, sperm count has previously been plausibly associated with environmental and lifestyle influences, including prenatal chemical exposure, adult pesticide exposure, smoking, stress and obesity. Therefore, sperm count may sensitively reflect the impact of the modern environment on male health across the lifespan and serve as a "canary in the coal mine" signaling broader risks to male health. [Original study.]
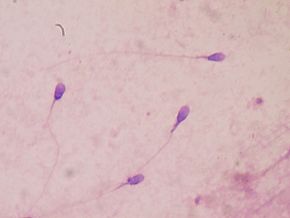
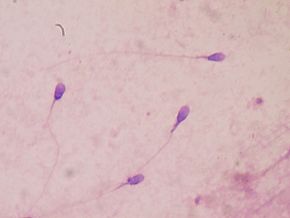 Human sperm. Credit: Wikipedia
Human sperm. Credit: Wikipedia
 Thunderstorm asthma? This is an asthma attack triggered by a thunderstorm - it is still relatively rare, but predicted to increase with the coming climate changes. During thunderstorms there are downdrafts of cold air which sweep up particles of pollens and mold spores into the clouds. There they absorb moisture and rupture into small, fragments (into a size easily inhaled into the lungs), which then are dispersed by rain and wind. When inhaled they can enter the lungs and trigger an asthma attack - thunderstorm asthma. [Note that normally larger pollen grains are usually filtered by hairs in the nose - so they don't make it to the lungs.] It seems that people with "hayfever" and allergies to grass pollen are at highest risk - at least in Australia. From Medscape:
Thunderstorm asthma? This is an asthma attack triggered by a thunderstorm - it is still relatively rare, but predicted to increase with the coming climate changes. During thunderstorms there are downdrafts of cold air which sweep up particles of pollens and mold spores into the clouds. There they absorb moisture and rupture into small, fragments (into a size easily inhaled into the lungs), which then are dispersed by rain and wind. When inhaled they can enter the lungs and trigger an asthma attack - thunderstorm asthma. [Note that normally larger pollen grains are usually filtered by hairs in the nose - so they don't make it to the lungs.] It seems that people with "hayfever" and allergies to grass pollen are at highest risk - at least in Australia. From Medscape:

 Psoriasis. Credit: Medscape
Psoriasis. Credit: Medscape Two more studies found that higher levels of vitamin D in the blood are associated with better health outcomes - one study found a lower risk of breast cancer, especially among postmenopausal women, and in the other - better outcomes after a metastatic melanoma diagnosis.
Two more studies found that higher levels of vitamin D in the blood are associated with better health outcomes - one study found a lower risk of breast cancer, especially among postmenopausal women, and in the other - better outcomes after a metastatic melanoma diagnosis. The
The 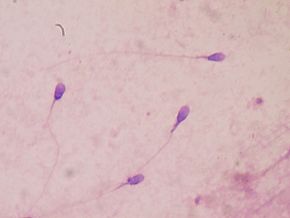 Once again a
Once again a  All of us at some point or another have wondered if we can hold on to medicines past their expiration date, or do we need to throw them out? And if they're still good past the expiration date, how much past the expiration date? Well... the investigative journalism site ProPublica has been examining this issue, and they published an article saying researchers and the government find that many medicines may be good for YEARS past the expiration date. Yes - years!
All of us at some point or another have wondered if we can hold on to medicines past their expiration date, or do we need to throw them out? And if they're still good past the expiration date, how much past the expiration date? Well... the investigative journalism site ProPublica has been examining this issue, and they published an article saying researchers and the government find that many medicines may be good for YEARS past the expiration date. Yes - years! The use of nanoparticles in foods is increasing every year, but we still know very little about whether they have health risks to humans, especially if one is eating foods with them daily (thus having chronic exposure). The
The use of nanoparticles in foods is increasing every year, but we still know very little about whether they have health risks to humans, especially if one is eating foods with them daily (thus having chronic exposure). The  Red meat allergies from a lone star tick bite? I first read about this a few years ago in
Red meat allergies from a lone star tick bite? I first read about this a few years ago in  Lone star tick Credit: CDC Public Image Library
Lone star tick Credit: CDC Public Image Library The following is a study with weird results, really weird results. And it makes me think of all the times I've heard people joke: "just smelling food makes me gain weight", because we all knew it wasn't true. But what if it was true? .... The results of this study done in mice are that actually smelling the food one eats results in
The following is a study with weird results, really weird results. And it makes me think of all the times I've heard people joke: "just smelling food makes me gain weight", because we all knew it wasn't true. But what if it was true? .... The results of this study done in mice are that actually smelling the food one eats results in