 Figured I'd post an article discussing a recent study that tested a new chronic sinusitis treatment, since so much of this site is devoted to sinusitis - both the latest research and treatments. Eh... I wasn't impressed with the study.
Figured I'd post an article discussing a recent study that tested a new chronic sinusitis treatment, since so much of this site is devoted to sinusitis - both the latest research and treatments. Eh... I wasn't impressed with the study.
Once again research was aimed at treating symptoms, rather than the actual microbial imbalance (dysbiosis) in the sinuses. No wonder it didn't work so well. The researchers added the corticosteroid drug budesonide to daily nasal saline irrigation in one group vs the other group just did daily nasal saline irrigation - both for 30 days. There were no statistically significant differences - both groups basically improved the same.
The researchers felt that the budesonide group "trended" toward more of an improvement, but statistically there wasn't a difference. The study was nicely done: it was double-blind (no one knew who got what), it had a placebo group (the saline irrigation only group), and people were randomly put into one or the other group. The budesonide (a corticosteroid) was meant as an alternative to, and to see if it was better than using a corticosteroid nasal spray - which many people with chronic sinusitis try for a while.
For those interested, here is the Sino-Nasal Outcome Test (SNOT-22) that people took before and after the 30 days of nasal irrigation, and which is used in many sinusitis studies. Note that some of the questions, in my mind, are bizarre as a measure of sinusitis symptoms and totally not appropriate, especially these 3 questions: Sad? Embarrassed? Frustrated/restless/irritable? And some of the questions are too vague. They list "post nasal drip" which is vague.
Where is a question about "mucus dripping down the throat", and even perhaps "gagging on mucus or phlegm" or "constantly clearing throat"? Where is "waking up with a daily sore throat"? How about "constant headaches", or "constantly feeling sick", or "need to sleep semi-sitting up"? These are descriptions people give me again and again. So eh... the test could use improvement.
Bottom line: People with chronic sinusitis have for years been doing nasal saline irrigation to help treat sinusitis symptoms. It helps the symptoms a little, but typically doesn't cure. From Medscape:
Does Budesonide Improve Outcome of Nasal Irrigation in Chronic Rhinosinusitis?
In patients with chronic rhinosinusitis (CRS), addition of budesonide to daily large-volume, low-pressure saline sinus irrigation might lead to improved outcome, but the findings are not clear-cut. ...continue reading "Adding Budesonide to Nasal Sinus Irrigation Does Not Help In Chronic Sinusitis"

 People ask me: what's going on with research in the treatment of sinusitis with probiotics? Well, the answer is that things are moving along slowly - very slowly, but there are good signs.
People ask me: what's going on with research in the treatment of sinusitis with probiotics? Well, the answer is that things are moving along slowly - very slowly, but there are good signs. Big announcement today! The high quality product
Big announcement today! The high quality product 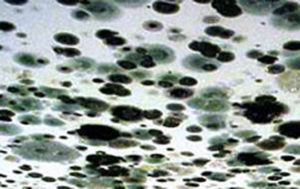 A number of people contacting me have indicated that living in a house or apartment with a mold problem led to their chronic sinusitis. And it wasn't the dreaded toxic black mold (varieties of mold which can cause serious neurological symptoms), but common molds that triggered their inflammatory reactions, respiratory symptoms, allergies, and eventually chronic sinusitis. All due to excessive mold exposure.
A number of people contacting me have indicated that living in a house or apartment with a mold problem led to their chronic sinusitis. And it wasn't the dreaded toxic black mold (varieties of mold which can cause serious neurological symptoms), but common molds that triggered their inflammatory reactions, respiratory symptoms, allergies, and eventually chronic sinusitis. All due to excessive mold exposure. An amazing new study is about to start in Sweden - this study will see if "snot transplants" work for the treatment for chronic sinusitis! Will this turn out to be a permanent treatment? While
An amazing new study is about to start in Sweden - this study will see if "snot transplants" work for the treatment for chronic sinusitis! Will this turn out to be a permanent treatment? While 
 Last week a person told an
Last week a person told an