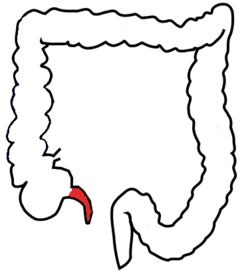
This is the second time I've seen research finding that antibiotics alone could be used (instead of surgery) for the treatment of uncomplicated appendicitis (June 17, 2015 post), but this time in children. Appendicitis is inflammation of the appendix. At the one year follow-up the researchers found that 75.7% of patients with uncomplicated appendicitis had been successfully treated with antibiotics alone and had not had any recurrences of appendicitis.
This is a major finding because for years the gold standard for appendicitis treatment has been an appendectomy. The times are a changing.
From Science Daily: Antibiotics alone can be a safe, effective treatment for children with appendicitis
Using antibiotics alone to treat children with uncomplicated acute appendicitis is a reasonable alternative to surgery when chosen by the family. A study led by researchers at Nationwide Children's Hospital found that three out of four children with uncomplicated appendicitis have been successfully treated with antibiotics alone at one year follow-up. Compared to urgent appendectomy, non-operative management was associated with less recovery time, lower health costs and no difference in the rate of complications at one year.
"Surgery has long been the 'gold standard' of care for treating appendicitis because by removing the appendix we eliminate the chance that the appendicitis will ever come back," said Dr. Deans. "However, early in our careers we noticed that patients with appendicitis who were placed on antibiotics overnight until their surgery the following morning felt better the next day. So, Pete and I asked ourselves: do they really need to have surgery?"
In the first study conducted and published in the United States examining non-operative management for appendicitis, they enrolled 102 patients age 7 to 17 who were diagnosed with uncomplicated acute appendicitis at Nationwide Children's between October 2012 and October 2013. Participants had early/mild appendicitis, meaning that they experienced abdominal pain for no more than 48 hours; had a white blood cell count below 18,000; underwent an ultrasound or CT scan to rule out rupture and to verify that their appendix was 1.1 centimeter thick or smaller; and had no evidence of an abscess or fecalith, which is hard stone-like piece of stool.
Thirty-seven families chose antibiotics alone and 65 opted for surgery. Those patients in the non-operative group were admitted to the hospital and received IV antibiotics for at least 24 hours, followed by oral antibiotics after discharge for a total of 10 days. Among those patients, 95% showed improvement within 24 hours and were discharged without undergoing surgery. Rates of appendicitis-related medical care within 30 days were similar between the groups with two patients in the non-operative group readmitted within 30 days for an appendectomy. At one year after discharge, three out of four patients in the non-operative group did not have appendicitis again and have not undergone surgery.
Appendicitis, caused by a bacterial infection in the appendix, is the most common reason for emergency abdominal surgery in children, sending more than 70,000 young people to the operating room each year. Although many of these cases are severe and require surgery, there are a good number that would be candidates for treatment with antibiotics alone, Dr. Minneci said.
According to the study results, patients who were transferred to Nationwide Children's from other institutions expressed concerns about the distance and time necessary to come back if the appendicitis recurred. These families opted for surgery more often. Patients whose families spoke primary languages other than English were more likely to choose antibiotics as a course of treatment due to cultural values to avoid surgery if at all possible.

 A large study found that using antidepressants during the second or third trimester of pregnancy increases the risk that the child will have autism by 87%, especially if the mother takes selective serotonin reuptake inhibitors (SSRIs). A drawback was that the study looked at associations rather than actual cause (which would have meant randomly assigning women to either treatment or no treatment - which is unethical). From Medical Xpress:
A large study found that using antidepressants during the second or third trimester of pregnancy increases the risk that the child will have autism by 87%, especially if the mother takes selective serotonin reuptake inhibitors (SSRIs). A drawback was that the study looked at associations rather than actual cause (which would have meant randomly assigning women to either treatment or no treatment - which is unethical). From Medical Xpress: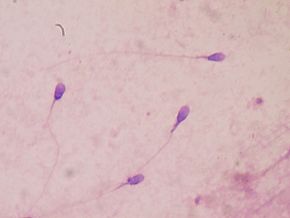 Recent research looked at environmental causes of male infertility, specifically endocrine-disrupting chemicals.
Recent research looked at environmental causes of male infertility, specifically endocrine-disrupting chemicals.


 It seems that a lot has been written about the health benefits of some berries, such as blueberries, while other berries have been neglected. This study focused on red raspberries, black raspberries, and blackberries. While the study was done in Poland, it was pointed out that these berries are also commonly grown in the USA. Red raspberry, black raspberry, and blackberry fruits are abundant in dietary phytochemicals such as flavonols, phenolic acids, ellagitannins, vitamins C and E, folic acid, and β-sitosterol. Many of these bioactive compounds exhibit antioxidant activity. Anthocyanins and other phenolic compounds such as ellagitannins and ellagic acid, which distinguish raspberry from other berries, occur in high levels and are mainly responsible for their broad beneficial health properties (including anti-inflammatory, antimicrobial, and antiviral activities).
It seems that a lot has been written about the health benefits of some berries, such as blueberries, while other berries have been neglected. This study focused on red raspberries, black raspberries, and blackberries. While the study was done in Poland, it was pointed out that these berries are also commonly grown in the USA. Red raspberry, black raspberry, and blackberry fruits are abundant in dietary phytochemicals such as flavonols, phenolic acids, ellagitannins, vitamins C and E, folic acid, and β-sitosterol. Many of these bioactive compounds exhibit antioxidant activity. Anthocyanins and other phenolic compounds such as ellagitannins and ellagic acid, which distinguish raspberry from other berries, occur in high levels and are mainly responsible for their broad beneficial health properties (including anti-inflammatory, antimicrobial, and antiviral activities). Reading this recent study, I was struck by how the results are evidence for eating sulforaphane containing foods, such as kale, cauliflower, brussels sprouts, broccoli, and cabbage for health and preventing cancer (due to anti-tumor activity). It is debatable whether it is support for taking supplements (here a sulforaphane supplement called BSE), even though the researchers were testing the supplement. Seven days of taking a supplement without "serious adverse events" (but they did have minor ones such as "mild abdominal discomfort") is too short a length of time for any support for a product. The real test would be seeing what health effects, both positive and negative, are after a year or two of taking the supplement.
Reading this recent study, I was struck by how the results are evidence for eating sulforaphane containing foods, such as kale, cauliflower, brussels sprouts, broccoli, and cabbage for health and preventing cancer (due to anti-tumor activity). It is debatable whether it is support for taking supplements (here a sulforaphane supplement called BSE), even though the researchers were testing the supplement. Seven days of taking a supplement without "serious adverse events" (but they did have minor ones such as "mild abdominal discomfort") is too short a length of time for any support for a product. The real test would be seeing what health effects, both positive and negative, are after a year or two of taking the supplement. Just a few years ago the type of pesticide (organophosphate, for example chlorpyrifos) looked at in this study was commonly used everywhere - in schools, homes, agriculture. It was easy to buy in stores (e.g., Raid spray), and was considered "safer" than older pesticides. Over time problem after problem has been found with them - with the latest being decreased lung function in children exposed to organophosphates early in life.
Just a few years ago the type of pesticide (organophosphate, for example chlorpyrifos) looked at in this study was commonly used everywhere - in schools, homes, agriculture. It was easy to buy in stores (e.g., Raid spray), and was considered "safer" than older pesticides. Over time problem after problem has been found with them - with the latest being decreased lung function in children exposed to organophosphates early in life. The mother is an important source of the first microbiome for infants by "seeding" the baby's microbiome - from the
The mother is an important source of the first microbiome for infants by "seeding" the baby's microbiome - from the