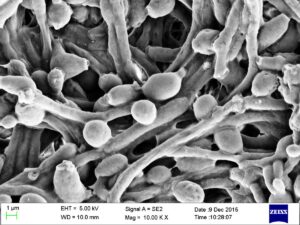
Not only humans and many foods (e.g., fruits) have microbiomes - the community of bacteria, viruses, archaea, and fungi living on and in the organism. Researchers found that trees also have microbiomes, and when a tree is diseased, the microbiome changes.
Not only humans and many foods (e.g., fruits) have microbiomes - the community of bacteria, viruses, archaea, and fungi living on and in the organism. Researchers found that trees also have microbiomes, and when a tree is diseased, the microbiome changes.
A single tree can be home to a trillion microbial cells! The microbes interact and depend on each other.
Additionally, different tree species have different microbiomes, and different parts of the tree have different microbiomes - the tree bark (sapwood) vs tree interior(heartwood). Makes sense!
Excerpts from NY Times: In Every Tree, a Trillion Tiny Lives
Scientists have found that a single tree can be home to a trillion microbial cells — an invisible ecosystem that is only beginning to be understood.
A forest is a complex, dynamic ecosystem in which a rich array of living things, from old-growth trees to microscopic fungi, interact and depend on one another for survival. ...continue reading "Every Tree Has A Microbiome"

 There has been discussion over the years regarding mouthwash - what are the harms and benefits? Does using
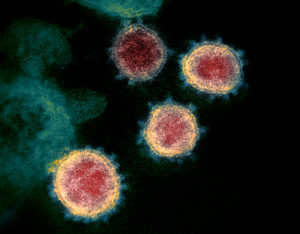
There has been discussion over the years regarding mouthwash - what are the harms and benefits? Does using  Millions of us have had a least one COVID infection. Many suffered a loss of smell during the infection. A recent
Millions of us have had a least one COVID infection. Many suffered a loss of smell during the infection. A recent 
 It is still unknown whether probiotic supplementation would help these conditions because the studies are not yet done. But researchers do suggest eating an anti-inflammatory diet - which means a diet rich in fruits, vegetables, whole grains, legumes (includes beans), fish, seeds, nuts, and olive oil. This kind of diet has lots of fiber to feed and support beneficial bacteria.
It is still unknown whether probiotic supplementation would help these conditions because the studies are not yet done. But researchers do suggest eating an anti-inflammatory diet - which means a diet rich in fruits, vegetables, whole grains, legumes (includes beans), fish, seeds, nuts, and olive oil. This kind of diet has lots of fiber to feed and support beneficial bacteria. Millions of pounds of pesticides are used each year in the US: on farms, in buildings and homes, on lawns, in pet flea and tick products - basically everywhere. And so the pesticides eventually wind up in us - from the foods we eat, the water we drink, the air we breathe (when pesticides drift during applications or when used indoors), and the treated lawns and ground we walk on.
Millions of pounds of pesticides are used each year in the US: on farms, in buildings and homes, on lawns, in pet flea and tick products - basically everywhere. And so the pesticides eventually wind up in us - from the foods we eat, the water we drink, the air we breathe (when pesticides drift during applications or when used indoors), and the treated lawns and ground we walk on. Exercise helps fight cancer. Wow! What a headline. But is it true?
Exercise helps fight cancer. Wow! What a headline. But is it true?
 Over the past decade there has been as increasing amount of research suggesting that the herpes virus (cold sores!) is implicated in the development of Alzheimer's disease. (
Over the past decade there has been as increasing amount of research suggesting that the herpes virus (cold sores!) is implicated in the development of Alzheimer's disease. (