 My last post was about a recent Medscape article discussing whether probiotics can be used to treat urinary tract infections (UTIs) (answer: probiotics are promising, but too little is known right now to recommend any). Two alternative treatments that the article did not discuss were drinking cranberry juice or taking cranberry supplements (studies are currently mixed regarding their effectiveness in UTIs - possibly due to varying cranberry products and doses used) and taking D-mannose supplements (whether as a powder or pill).
My last post was about a recent Medscape article discussing whether probiotics can be used to treat urinary tract infections (UTIs) (answer: probiotics are promising, but too little is known right now to recommend any). Two alternative treatments that the article did not discuss were drinking cranberry juice or taking cranberry supplements (studies are currently mixed regarding their effectiveness in UTIs - possibly due to varying cranberry products and doses used) and taking D-mannose supplements (whether as a powder or pill).
D-mannose is recommended on alternative medical sites as an effective treatment for UTIs caused by E.coli, including recurrent UTIs. Studies show that up to 90% of UTIs are caused by E. coli.The majority of both males and females writing comments about UTI treatments on these sites and for D-mannose product reviews (on Amazon) rave about D-mannose as the only treatment that worked for them after suffering from recurrent UTIs (antibiotics typically did not work well for them).
D-mannose is a naturally occurring sugar found in a number of fruits, especially cranberries and blueberries. D-mannose is effective because it attaches to E. coli bacteria, and prevents them from attaching to the walls of the urinary tract. (Researchers write that D-mannose "inhibits bacterial adhesion to uroepithelial cells.") Persons taking D-mannose are also advised to drink plenty of water, which then flushes out the bacteria.
The typical dose of D-mannose for UTI treatment is 500 mg, in capsule or powder form, taken in a glass of water or juice, every few hours for five days (perhaps 5 or 6 tablets a day). Then continue taking for a few days after all symptoms go away to make sure all the bacteria are flushed out of the urinary tract.
Many long-term recurrent UTI sufferers continue taking D-mannose at lower doses to prevent the UTIs from recurring. There are no known side-effects. D-mannose is easily found at grocery stores, health food stores, and online.
After doing a D-mannose and urinary tract infection search using PubMed (from Medline, the National Institute of Health), I found that currently there is only one published study looking at the use of D-Mannose in urinary tract infections.
The 2014 study by B. Kranjcec, D. Papes, and S. Altarac looked at the effectiveness of D-mannose powder for recurring urinary tract infections in women. 308 women with a history of recurrent UTIs were first treated with an antibiotic (ciprofloxacin) for an UTI, and then were randomly assigned to one of 3 groups for 6 months. The 3 groups were: D-mannose (2 g of D-mannose in 200 ml water daily), or prophylactic antibiotics (50 mg Nitrofurantoin daily) or a control group that didn't take anything (no prophylaxis).
Results were that 98 patients (31.8%) had a recurrent UTI. Of those 98, 14.6% (15 women) were in the D-mannose group, 20.4% (21 women) in the Nitrofurantoin antibiotic group, and 60.8% (62 women) in the no treatment (no prophylaxis) group. In other words, the D-mannose group did the best in preventing recurrences, even better than the antibiotic.
From World Journal of Urology: D-mannose powder for prophylaxis of recurrent urinary tract infections in women: a randomized clinical trial.
Overall 98 patients (31.8%) had recurrent UTI: 15 (14.6) in the D-mannose group, 21 (20.4) in Nitrofurantoin group, and 62 (60.8) in no prophylaxis group, with the rate significantly higher in no prophylaxis group compared to active groups (P < 0.001). Patients in D-mannose group and Nitrofurantoin group had a significantly lower risk of recurrent UTI episode during prophylactic therapy compared to patients in no prophylaxis group (RR 0.239 and 0.335, P < 0.0001). In active groups, 17.9% of patients reported side effects but they were mild and did not require stopping the prophylaxis. Patients in D-mannose group had a significantly lower risk of side effects compared to patients in Nitrofurantoin group (RR 0.276, P < 0.0001), but the clinical importance of this finding is low because Nitrofurantoin was well tolerated.

 Amusing but also scary. The negative effects on the gut microbes of one person consuming an all fast food diet for 10 days occurred very quickly, and his gut microbes did not recover even 2 weeks after the fast food diet ended. Biggest problem seemed to be loss of gut diversity - about 40% of his gut bacterial species. Loss of gut diversity is considered a sign of ill health. Written by Tim Spector, with Tom Spector's assistance, from The Conversation:
Amusing but also scary. The negative effects on the gut microbes of one person consuming an all fast food diet for 10 days occurred very quickly, and his gut microbes did not recover even 2 weeks after the fast food diet ended. Biggest problem seemed to be loss of gut diversity - about 40% of his gut bacterial species. Loss of gut diversity is considered a sign of ill health. Written by Tim Spector, with Tom Spector's assistance, from The Conversation:
 Tom Spector. Credit: Tim Spector
Tom Spector. Credit: Tim Spector
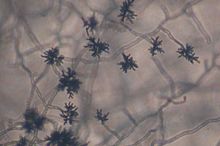
 Guess what? Our microbiome (the collection of microbes living within and on us) also normally contains fungi. This is our mycobiome. Very little is known about the mycobiome. (in contrast, much, much more is known about the bacteria within us) The fungi within us may be as low as 0.1% of the total microbiota (all our microbes). But what is known is because advanced genetic analyses have been done (specifically "next-generation” sequencing") or culturing of the fungi.
Guess what? Our microbiome (the collection of microbes living within and on us) also normally contains fungi. This is our mycobiome. Very little is known about the mycobiome. (in contrast, much, much more is known about the bacteria within us) The fungi within us may be as low as 0.1% of the total microbiota (all our microbes). But what is known is because advanced genetic analyses have been done (specifically "next-generation” sequencing") or culturing of the fungi.
 Every time you inhale, you suck in thousands of microbes. And depending on where you live, the microbes will vary. From Wired:
Every time you inhale, you suck in thousands of microbes. And depending on where you live, the microbes will vary. From Wired: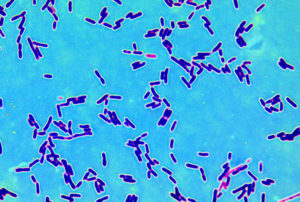 This nice general summary of what scientists know about the microbial community within us was just published by a division of the NIH (National Institutes of Health). Very simple and basic. From the National Institute of General Medical Sciences (NIGMS):
This nice general summary of what scientists know about the microbial community within us was just published by a division of the NIH (National Institutes of Health). Very simple and basic. From the National Institute of General Medical Sciences (NIGMS): A
A