Again, the same message of what are healthy habits to prevent heart attacks and heart disease: not smoking, a normal body mass index, physical activity of at least 2.5 hours per week, watching seven or fewer hours of television a week, consumption of a maximum of one alcoholic drink per day on average, and a diet in the top 40 percent of a measure of diet quality.From Medical Xpress:
A healthy lifestyle may prevent heart disease in nearly three out of four women
A new study that followed nearly 70,000 women for two decades concluded that three-quarters of heart attacks in young women could be prevented if women closely followed six healthy lifestyle practices.
The study, published today in the Journal of the American College of Cardiology, followed participants in a study of nurses established in 1989, which surveyed more than 116,000 participants about their diets and other health habits every two years. Researchers from Indiana University, the Harvard School of Public Health, and Brigham and Women's Hospital analyzed data on 69,247 of the participants who met the requirements for their study. "Although mortality rates from heart disease in the U.S. have been in steady decline for the last four decades, women aged 35-44 have not experienced the same reduction," said Andrea K. Chomistek, ScD, a researcher from the Indiana University School of Public Health-Bloomington and lead author of the paper.
Healthy habits were defined as not smoking, a normal body mass index, physical activity of at least 2.5 hours per week, watching seven or fewer hours of television a week, consumption of a maximum of one alcoholic drink per day on average, and a diet in the top 40 percent of a measure of diet quality based on the Harvard School of Public Health healthy eating plate.
During 20 years of follow-up, 456 women had heart attacks and 31,691 women were diagnosed with one or more cardiovascular disease risk factors, including type 2 diabetes, high blood pressure or high levels of blood cholesterol. The average age of women in the study was 37.1 years at the outset; the average age of a heart disease diagnosis was 50.3, and the average age for diagnosis with a risk factor for heart disease was 46.8.
Researchers found that women who adhered to all six healthy lifestyle practices had a 92 percent lower risk of heart attack and a 66 percent lower risk of developing a risk factor for heart disease. This lower risk would mean three quarters of heart attacks and nearly half of all risk factors in younger women may have been prevented if all of the women had adhered to all six healthy lifestyle factors, the authors said.
Independently, not smoking, adequate physical activity, better diet, and lower BMI were each associated with a lower risk for heart disease. Women who consumed moderate amounts of alcohol—approximately one drink per day on average—saw the lowest risk compared to those who did not drink at all and those who drank more.

 Another excellent reason to start walking more and increasing daily physical activity. So get out there and walk, walk, walk...
Another excellent reason to start walking more and increasing daily physical activity. So get out there and walk, walk, walk... Take note: the focus should be on getting magnesium from foods, not supplements. As the researchers warn: "your body absorbs magnesium from food differently than it does from supplements". From CNN:
Take note: the focus should be on getting magnesium from foods, not supplements. As the researchers warn: "your body absorbs magnesium from food differently than it does from supplements". From CNN: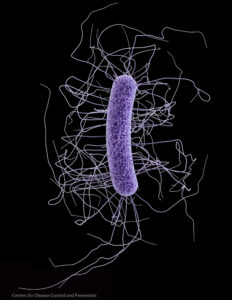 Clostridium difficile. Credit: CDC
Clostridium difficile. Credit: CDC Once again air pollution is linked to health problems, this time exposure during pregnancy is linked to congenital malformations (what are commonly called birth defects). From Science Daily:
Once again air pollution is linked to health problems, this time exposure during pregnancy is linked to congenital malformations (what are commonly called birth defects). From Science Daily: