About 300,000 people are diagnosed with Lyme disease every year, according to new estimates from the Centers for Disease Control and Prevention (CDC). Lyme disease is caused by bacteria that multiply in the bodies of ticks, people and animals, including mice, deer and dogs.... the tiny blacklegged deer tick, which is the most common transmitter of Lyme disease.
These deer ticks pick up Lyme bacteria (Borrelia burgdorferi) when they feed on the blood of infected mice, chipmunks and other hosts. Infected ticks in both the nymphal and adult life stages can then transfer the Lyme bacteria to humans if they latch on for a meal and feed for approximately 36 hours or more. Lyme disease is highly treatable when it’s detected early, but devastating when the infection goes unnoticed for more than a few months.
Let Poultry Help with Tick Prevention Leafy wooded areas and grassy meadows are the preferred habitats for blacklegged deer ticks and American dog ticks, which both spend their larval stage in leaf litter, their nymphal stage on small animals, and their adult stage in tall grass or other shrubby vegetation. People have learned how to get rid of ticks by keeping foraging chickens and guinea fowl on their property. In April 2015, we launched the MOTHER EARTH NEWS Chickens and Ticks Survey, and responses revealed that: 71 percent had an existing tick problem before they got poultry, 78 percent kept poultry that helped control or eliminate ticks within the birds’ feeding range, 46 percent experienced a drop in tick populations within a month after getting poultry; 45 percent saw good control after several months to a year.Many respondents noted that small bantam chickens and game hens can get into tight spots where larger birds can’t fit, resulting in better tick control....
Permethrin-Treated Clothes and ‘Tick Tubes’ If you live in one of the 13 states where Lyme disease risk is highest, learning how to get rid of ticks should be a top priority. You might want to consider using permethrin, a non-organic pesticide that repels and kills ticks. Permethrin is more potent and persistent than the organic materials we usually recommend. We suggest using a formula designed to be applied to clothing rather than misters, sprayers, foggers or other permethrin products. Clothing products that are pre-treated with permethrin are available, or you can buy permethrin with instructions for how to use it to treat your clothes. Take care to not expose kids to this pesticide...The EPA also classified permethrin as “likely to be carcinogenic to humans,” so weigh the risk of infrequent exposure to the risk of Lyme disease in your area.
You might also consider permethrin-infused “tick tubes,” which are designed to kill ticks on white-footed mice as well as chipmunks and rats, the main animals from which ticks become infected with Lyme. The tick tubes offer nesting materials impregnated with the pesticide to such critters. The animals then take the material back to their nests, where it kills any ticks that may have latched on to the adults and their young. The small amount of permethrin used in tick tubes is not water-soluble, so it’s not likely to end up anywhere but in a nest. Sold commercially as Damminix Tick Tubes, these devices are easy to make yourself....
Herbal Tick Repellents Many of our survey respondents reported that they apply veterinary-prescribed tick preventatives on their dogs and cats, but would prefer more organic repellents. Two plant-based aromatics — sweet-scented “rose” geranium (Pelargonium graveolens) essential oil and eastern red cedar (Juniperus virginiana; also known as “red cedarwood”) essential oil — were repeatedly recommended by readers who use them as spray-on repellents for pets and family members alike....Both geranium essential oil and eastern red cedar essential oil have proven to be successful repellents against ticks in various life stages, according to the Journal of Agricultural and Food Chemistry and the Journal of Medical Entomology, respectively.
Using full-strength essential oil can injure human skin and overwhelm pets’ sensitive noses, so follow this simple recipe when making a liquid anti-tick spray: In an 8-ounce spray bottle, combine 10 to 20 drops of rose geranium or eastern red cedar essential oil with 1 teaspoon of vodka or rubbing alcohol. Fill the rest of the bottle with water and shake to combine. The spray can be applied to your skin or clothing....
More Tick Prevention Tricks Fencing out deer, the primary host of adult Lyme-infected ticks, can help prevent ticks from reaching your land. Low-cost, plastic-mesh deer fencing is available online and at farm stores. Ticks rarely inhabit lawns that are mowed regularly. Raking up leaves and composting them deprives overwintering ticks of shelter.
When hiking where tick populations are high, stay on the trails and dress defensively — pull your socks up over your pants. When only shorts will do, some people cut off the ankle sections of old socks, spray them with a repellent, and wear the tubes around their calves like tick-deterring leg warmers.
A study published in Experimental and Applied Acarology found that spraying outdoor areas with Safer-brand organic insecticidal soap in spring, when blacklegged deer tick nymphs are active, can provide treatment that is equally as effective as spraying with the insecticide chlorpyrifos.
After you’ve been outdoors, check your dogs for any ticks that may have latched on, and then make your way to a hot, soapy shower followed by a careful body check. You can kill any ticks that have attached to your clothing by immediately putting your clothes into the dryer for 15 minutes on the hottest setting, and then washing them. Most ticks are sensitive to dry heat, but may survive even the hottest wash.
 It's official - the medical community has accepted that a key element in preventing allergies and asthma is early childhood exposure to allergens - whether peanuts, dust, or pets. Instead of avoiding the allergens (which was the medical advice for decades) - getting early exposure to them is key to preventing allergies. Apparently growing up on a farm is best (with exposure to farm dirt and dust), especially a dairy farm with animals and raw milk (a number of studies have found that unprocessed raw milk and its microbes also helps health). But if one doesn't live on a farm, then having furry pets in early childhood is also beneficial in reducing the incidence of allergies. The following study shows that microbes are involved - pet microbes were found in the guts of many of those children who did not develop early allergies! From Medscape:
It's official - the medical community has accepted that a key element in preventing allergies and asthma is early childhood exposure to allergens - whether peanuts, dust, or pets. Instead of avoiding the allergens (which was the medical advice for decades) - getting early exposure to them is key to preventing allergies. Apparently growing up on a farm is best (with exposure to farm dirt and dust), especially a dairy farm with animals and raw milk (a number of studies have found that unprocessed raw milk and its microbes also helps health). But if one doesn't live on a farm, then having furry pets in early childhood is also beneficial in reducing the incidence of allergies. The following study shows that microbes are involved - pet microbes were found in the guts of many of those children who did not develop early allergies! From Medscape:

 Yes, even healthy newborns have a diversity of viruses in the gut - this is their
Yes, even healthy newborns have a diversity of viruses in the gut - this is their  [UPDATE: I added an Oct. 2018 update to the post
[UPDATE: I added an Oct. 2018 update to the post  Another article from results of the crowdsourced study in which household dust samples were sent to researchers at the University of Colorado from approximately 1200 homes across the United States. Some findings after the dust was analyzed: differences were found in the dust of households that were occupied by more males than females and vice versa, indoor fungi mainly comes from the outside and varies with the geographical location of the house, bacteria is determined by the
Another article from results of the crowdsourced study in which household dust samples were sent to researchers at the University of Colorado from approximately 1200 homes across the United States. Some findings after the dust was analyzed: differences were found in the dust of households that were occupied by more males than females and vice versa, indoor fungi mainly comes from the outside and varies with the geographical location of the house, bacteria is determined by the  This is a nice study showing cause and effect: 6 hours of sleep or less at night lowers the body's resistance so that the person is more likely to catch a cold virus. From Science Daily:
This is a nice study showing cause and effect: 6 hours of sleep or less at night lowers the body's resistance so that the person is more likely to catch a cold virus. From Science Daily: I recently posted on ways the number of
I recently posted on ways the number of  This article discusses the fungi living on our skin. Recent research (using state of the art genetic analysis) has found that healthy people have lots of diversity in fungi living on their skin. Certain areas seem to have the greatest populations of fungi:
This article discusses the fungi living on our skin. Recent research (using state of the art genetic analysis) has found that healthy people have lots of diversity in fungi living on their skin. Certain areas seem to have the greatest populations of fungi: 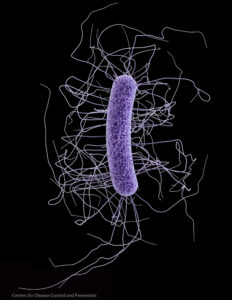 More research that supports that both more variety (diversity) of microbes and the actual mix of types of microbes are involved in a healthy
More research that supports that both more variety (diversity) of microbes and the actual mix of types of microbes are involved in a healthy  There has been much discussion recently about breastfeeding - why is it so important? Is it really better than formula? The answer is: YES, breastfeeding is the BEST food for the baby, and for a number of reasons. Not only is it nature's perfect food for the baby, but it also helps the development of the baby's microbiome or microbiota (the community of microbes that live within and on humans).
There has been much discussion recently about breastfeeding - why is it so important? Is it really better than formula? The answer is: YES, breastfeeding is the BEST food for the baby, and for a number of reasons. Not only is it nature's perfect food for the baby, but it also helps the development of the baby's microbiome or microbiota (the community of microbes that live within and on humans).